In 2020, 13% of people age 50 to 80 delayed getting medical care due to being worried about cost. And 12% who actually needed medical care didn’t get it because they couldn’t afford it.
And it doesn’t stop there. People are worried about paying medical bills in 2022. In fact, 18% of the people were doubtful they’d be able to pay for their healthcare expenses next year.
That’s according to the University of Michigan National Poll on Healthy Aging. It surveyed a national sample of adults aged 50-80 about their concerns affording needed health care.
How can older adults fix this?
Older adults can help solve this problem by saving money in tax-advantage accounts like:
- health savings account
- flexible spending accounts (FSAs), and
- health reimbursement arrangements (HRAs).
These programs can be used to pay out-of-pocket healthcare expenses.
Health savings accounts
Health savings accounts (HSA) can help older people afford the care they need. People can put money in the HSA account on a pre-tax basis to pay for qualified medical costs. Firms can also contribute pre-tax dollars up to an annual limit. Money that’s put in and taken out is not taxed. And this money rolls over from year to year.
High-deductible health plans (HDHP) qualify an employee for an HSA. According to the poll, to qualify as a HDHP in 2021 for a single person it’s $1,400 and for a family it’s $2,800.
But of the people who responded, only 7% had an HSA. And among the 21% who had a HDHP, only 45% had an HSA.
Also, it was more common for people in the 50-64 age range (12%) to have an HSA, than compared to people 65-80 (1%). And people with at least a bachelor’s degree were more likely to have one (13%) than those with a high school or less education (3%). Finally, 13% of respondents with household incomes of at least $100,000 had an HSA compared to less than 2% of those with a household income of $30,000.
Flexible spending accounts
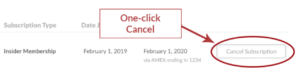
Flexible Spending Accounts (FSAs) also allow employees to set aside pre-tax dollars to use reimbursement for out-of-pocket healthcare expenses. However, this money doesn’t rollover. FSA are a use-it-or-lose-it plan. Whatever remains at the end of the year is forfeited.
Only 12% of people in the study said they had an FSA. Those who did were more often in the 50–64 (12%), had at least a bachelor’s degree (18%), and had annual household incomes of at least $100,000 (22%).
Health reimbursement arrangements
Health reimbursement arrangements (HRAs) are employer-owned, employer-funded group health plans. Employees get reimbursed tax-free for qualified medical expenses from HRAs. However, there’s a cap off on the amount they can be reimbursed per year. And while unused money can be rolled over from year to year, the money that’s in the account is owned by the employer.
Only 5% of people in the study said they had an HRA. Those who did, however, had at least a bachelor’s degree (6%), an annual household income of at least $100,000 (7%) and were in excellent, very good or good physical health (5%).
Takeaway
The sad truth to what this study shows: Many older people are worried about heathcare costs, but few are saving money for it.
Why? Because they can’t afford to.
This presents an opportunity for Benefits pros to help them out. Educate them on what HSAs, FSAs and HRAs are, how they can help them and how they can use them.
Targeting these groups and providing easy-to-understand info, can keep these employees healthier and in the long run cut down on your company’s healthcare costs.